Bradycardia (from the Greek βραδύς=slow, and καρδία=heart) is the most common appearance of a conduction system disease. Indeed, any disease involving either the onset or the propagation of the cardiac electrical activity may result in a severe bradycardia, that is, a rhythm slower than 40 bpm.
BradyArrhythmias causes may be
- a defect of impulse output within the Sino-Atrial Node, termed as Sick Sinus Syndrome (SSS)
- a defect in impulse conduction across the Atrio-Ventricular Node (AVN), termed as Atrio-Ventricular Block (AVB)
- a defect in impulse conduction across the His-Purkinje system, termed as Atrio-Ventricular Block (AVB). This latter AVB is usually more severe than a block in the AVN.
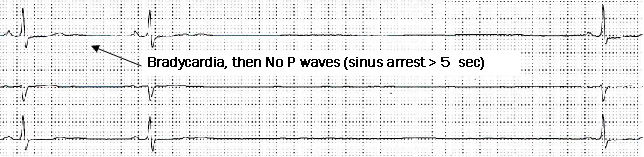
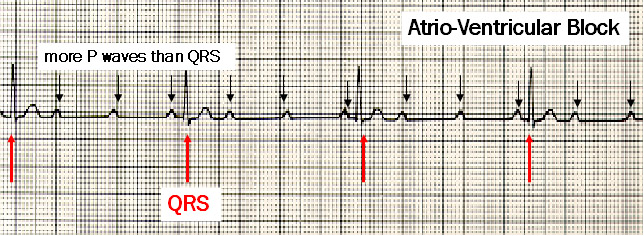
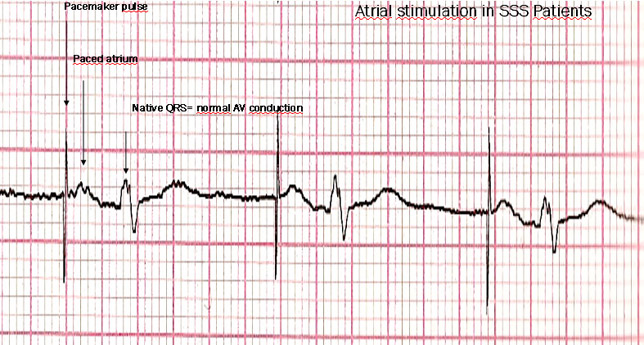
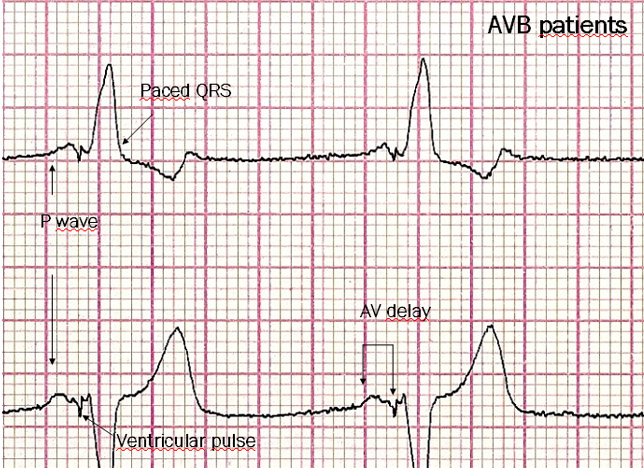
In SSS patients the EKG pattern is a slow heart rate (HR) with a few P waves, whereas in AVB conduction from the atria to the ventricles is disrupted, hence P waves outnumber QRS complexes.
A finding common to all BradyArrhythmias is a slow HR that does not increase with exercise as in normal subjects: fatigue, breathlessness, and palpitation are the symptoms of this clinical picture. In the most severe cases, pauses of the cardiac activity may suddenly occur, causing absence of cardiac muscle contraction. Transient hypotension ensues, with symptoms of light-headedness or syncope (transient loss of consciousness) when pauses exceeding 8 seconds occur. The tolerance to hypotension may vary, depending on age, underlying heart disease and body position. Consciousness is usually maintained for a longer time when lying supine.
EKG patterns of BradyArrhythmias
SSS: a slow HR (< 45 bpm) with a few P waves or no P waves is observed. Pauses or prolonged cardiac arrest (from 2 up to 10 seconds) are also common findings. The HR usually does not increase, or increases poorly during exercise.
AVB: conduction of the P waves to the ventricles is failing, hence more P waves than QRS are observed.
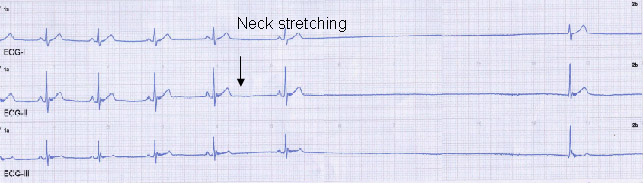
A peculiar condition is Neurally Mediated Syncope: a transient loss of consciousness may occur based on an abnormal reflex that stops suddenly the heart rhythm, and may also cause a blood pressure drop. The reflex onset is most commonly located in the carotid artery receptors, whose compression/stretching elicits cardiac arrest and hypotension. The cardiac electric system is usually normal in 80% of cases.
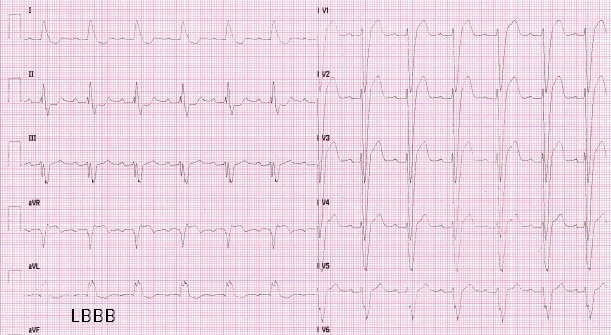
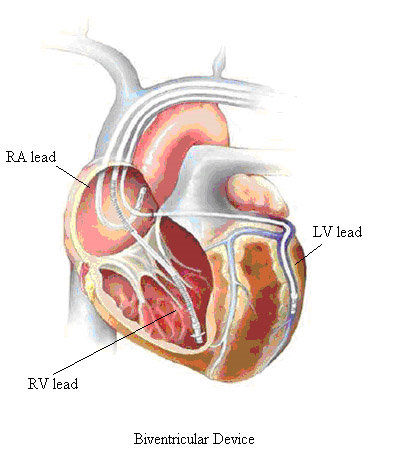
Heart Failure due to Left Ventricular (LV) systolic dysfunction is worsened when a Left Bundle Branch Block (LBBB) coexists, owing to an uncoordinated LV contraction. Cardiac resynchronization Therapy (CRT) achieved by LV stimulation may greatly benefit this subset of patients.
BradyArrhythmias Symptoms
Whatever the specific disease of the cardiac electric system, symptoms are related to the type and to the severity of bradycardia:
- Sudden cardiac pauses cause light-headedness or transient loss of consciousness (syncope) depending on the duration of the pause. Syncope occurs with pauses > 8 seconds
- Severe bradycardia causes fatigue, breathlessness, palpitation, inability to exercise. Indeed, cardiac output cannot increase owing to a low HR, such that a normal lifestyle is not possible.
BradyArrhythmias Treatment
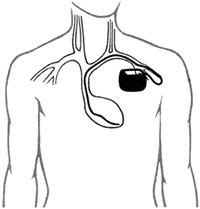
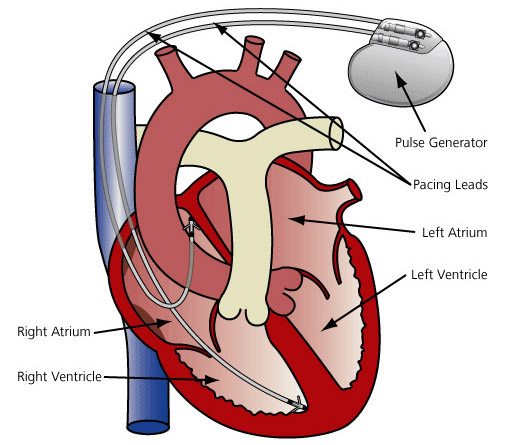
Cardiac stimulation by a Pacemaker benefits all the patients symptomatic because of Bradyarrhythmias. Pacemakers consist of a Pulse Generator (microprocessor + battery) and one or more leads. The leads are implanted inside the heart (endocardial leads) or on its outer layer (epicardial leads).
What is the Pacemaker function ?
SSS: since the disease is a poor P wave output in the Sino-Atrial node, the pacemaker elicits a pulse to the atrial muscle any time the HR drops down to the programmed rate.
AVB: P waves are not conducted to the ventricles. The Pacemaker detects the P wave, then an Atrio-Ventricular (AV) timing is started. In the event this AV delay times out in the absence of a native QRS, a ventricular pulse is delivered.
Where both a poor P wave output and AVB coexist, atrial and ventricular stimulation occur. Rate-Responsive pacemakers can increase the HR according to a specifically programmed setting in the event the patient’s rhythm is chronothropically incompetent.

About the Leads.
Leads consist of two metallic wires coated by an insulating sheath. The conductors allow the CIEDs to detect the intrinsic activity of the heart, and to provide electrical stimulation.
The Right Ventricular leads of cardioverter-defibrillators (ICDs) have 3 to 4 conductors: one (single coil lead) or two (dual coil lead) conductors are coiled as to provide a large-area electrode to deliver the high-voltage pulse (termed “shock”) needed to terminate fast arrhythmias.
Single chamber devices need a single lead, most frequently to pace the ventricle. Dual chamber devices have both an atrial and a ventricular lead to detect the signal and pace either cardiac chamber. Biventricular devices are equipped with 3 leads. Examples of all these settings are reported below.
Single Chamber Ventricular Device
Dual Chamber Pacemaker