Tachycardia (from the Greek ταχύς=fast, and καρδία=heart) means a fast Heart Rate (HR) that is the common appearance of non-physiologic abnormal Rhythms. Differently from Sinus Tachycardia, that is the normal HR increase related to exercise or stressful events, TachyArrhythmias arise outside the Sino-Atrial Node.
Albeit Tachycardia is the hallmark of any fast arrhythmia, a distinction needs to be made between Supraventricular Tachycardias and Ventricular Tachycardias. Indeed, Ventricular Tachycardias are more commonly associated to a structural heart disease and have a more complex therapeutic approach.
The vast majority of Supraventricular Tachycardias arising at specific anatomical sites such as Atrial Flutter, Ectopic Atrial Tachycardias, and Atrio-Ventricular Reciprocating Tachycardias are nowadays treated by substrate ablation or drugs.
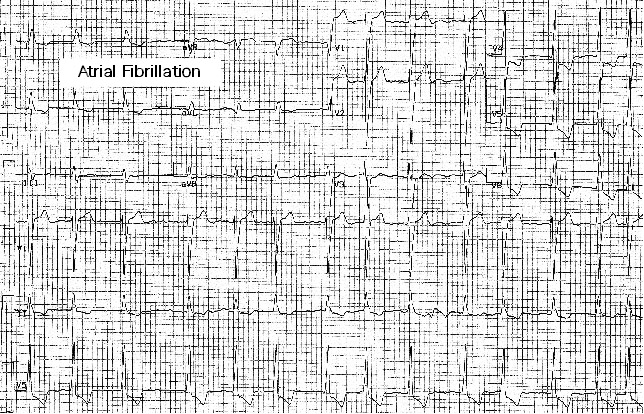
The most important Supraventricular Arrhythmia in clinical practice is Atrial Fibrillation, since it is a major predisposing factor to ischemic stroke, may cause disabling symptoms and precipitate heart failure, and is quite common in the ageing population. Atrial Fibrillation (AF) may pose a significant interaction with patients receiving device therapy, as it occurs in about 30% of pacemaker (PM) or implantable cardioverter-defibrillator (ICD) patients. Inappropriate delivery of ICD therapy or misclassification of a ventricular tachycardia because of AF are the main unwanted outcomes in ICD patients.
Ventricular TachyArrhythmias arise in the ventricles, and are clinically relevant when causing symptoms: transient loss of consciousness, lightheadedness, chest pain, breathlessness, fatigue, palpitation. They are usually classified as:
Monomorphic Ventricular Tachycardia (MVT).
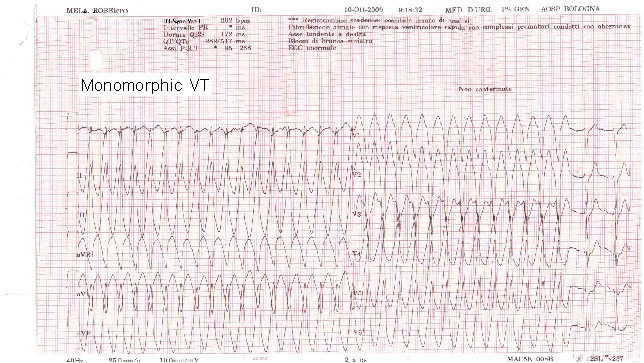
Regular rhythm with reproducible morphology. The heart rate has a wide range, from 110 to 250 bpm. MVT causes a decrease of cardiac output and of blood pressure depending on the underlying heart disease and on the heart rate. Symptoms may range from moderate to severe, up to cardiac arrest.
Polimorphic Ventricular Tachycardia (PVT).
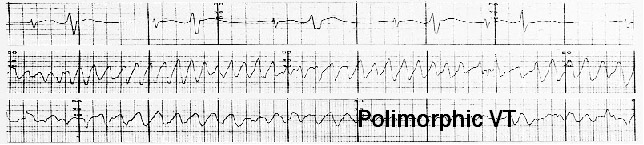
Both heart rate and tachycardia morphology are unstable. The HR is usually very fast (>200 bpm). High chances of degeneration into Ventricular Fibrillation (VF), but spontaneous termination may occur.
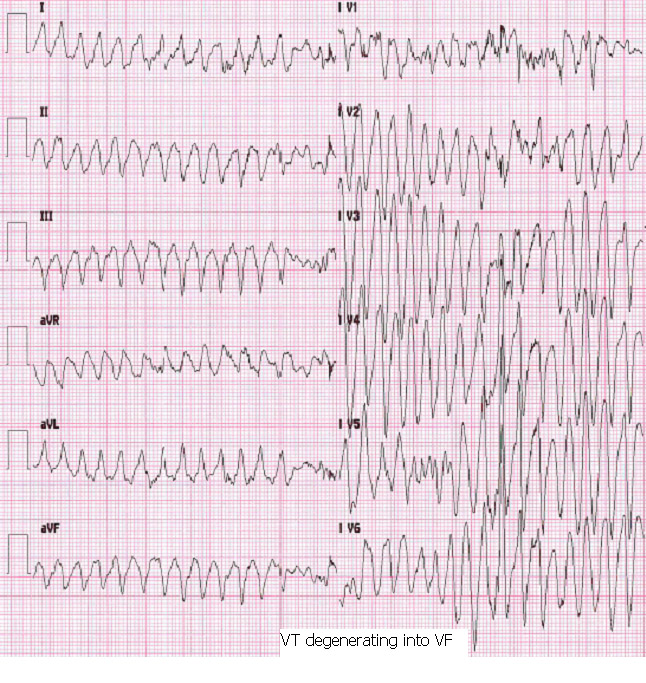
Ventricular Fibrillation (VF).
Completely irregular rhythm, HR > 250 bpm, morphology hardly detectable. Frequently triggered by a PVT or a MVT. Symptoms usually severe, spontaneous termination unlikely.
Ventricular TachyArrhythmias may arise in a wide spectrum of clinical settings, ranging from the acute phase of a myocardial infarction to Cardiomyopathies to genetic abnormalities of ion channels in the absence of a structural heart disease. Such an heterogeneity of clinical settings means an extremely different risk of arrhythmia occurrence, and makes the clinical approach a strictly tailored one.
Prevention of Ventricular arrhythmias by tailored interventions (lifestyle and behavioural changes, treatment of associated heart disease or co-morbidities, pharmacologic counselling, drug administration) may be a first step in subjects whose clinical history portends the risk of arrhythmias, whereas Therapeutic Interventions are usually taken for those who already have experienced Ventricular TachyArrhythmias.
Beyond those abovementioned for Prevention, Ablation of the arrhythmia substrate and the Implantable Cardioverter-Defibrillator (ICD) are helpful interventions to treat patients at risk of recurrent Ventricular TachyArrhythmias that do not have a transient and correctable cause.
When is an ICD recommended in clinical practice ?
- To terminate Ventricular Tachycardias and Ventricular Fibrillation in subjects who already have experienced cardiac arrest or poorly tolerated Ventricular TachyArrhythmias in the absence of a transient and correctable cause. In these patients the ICD is the most effective intervention to prevent sudden cardiac death (SCD). These subjects are considered candidates to ICD therapy for Secondary Prevention of SCD.
- To prevent sudden cardiac death in subjects that have not experienced ventricular TachyArrhythmias yet, but are deemed at risk based on their clinical profile and history, and in whom the value of other preventative strategies is not warranted as sufficient. These patients are considered candidates to ICD therapy as the Primary Prevention of SCD.